One of the biggest current challenges to public health are the perils to human health and health system attributable to climate change. The impact on different age groups and genders are varied. Environmental alterations result in respiratory and zoonotic diseases. There is urgent need for coordinated activities to combat this challenge.
Introduction
Climate change, as per the United Nations Climate Action panel, refers to long-term shifts in temperatures and weather patterns of the earth1. On a smaller scale, this is a part of natural phenomena; however, humans have intensified these alterations by increased burning of fossil fuels. This emanates greenhouse gases like carbon dioxide, which remain in the atmosphere, thereby trapping the Sun’s heat and raising mean temperatures1.
In the Twenty First century, the temperature of the earth is about 1.1◦C warmer than that in the late 1800s1. Apart from warmer temperatures, consequences of climatic variability also include droughts, fires, rising sea levels, floods, hurricanes and diminishing biodiversity1. In this review article, an attempt has been made to explain the effects of varying climate patterns on health outcomes and health systems using the WHO framework given below.
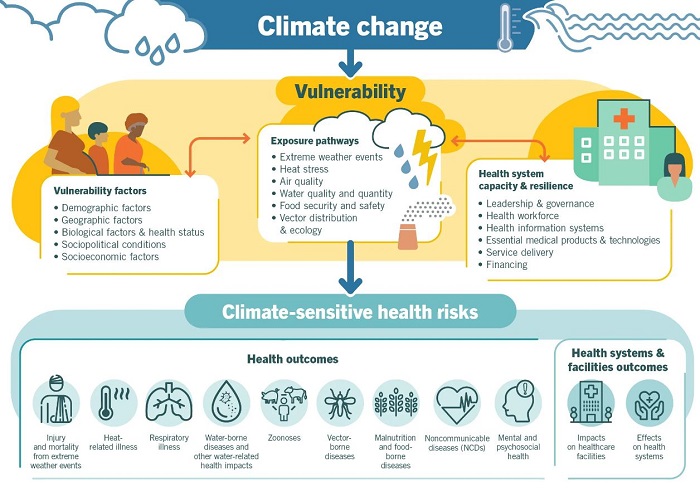
Figure 1: The WHO framework health effects of climate change2 as depicted in the article “Climate Change and Health” on 30 Oct, 2021 [https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health]
As the framework is extensive, the authors decided to discuss only a few selected factors. Selection has been made based on their relevance from policy action point of view. Demographic factors, Air Quality and Health service delivery are selected from the vulnerability, exposure pathways and health system capacity respectively. Health risks are studied under zoonotic diseases and Respiratory illnesses and lastly, the health systems outcome will also be examined.
Demographic patterns
People who are least responsible for the greenhouse gas emissions are the most vulnerable to the adverse effects of climate change. Pertinent examples include people living in low-and-middle income countries (LMIC), those in Island nations, mountains, coastal and Polar Regions.
Gender analysis indicated that the probability of women dying in heat waves and due to cyclones (in Bangladesh and Philippines) is greater compared to males3. They are also the prime victims of food shortage, partner violence, mental health issues, and poor reproductive and maternal health3. It is also noted that the incidence of preeclampsia, uterine bleeding and low birth weight babies are increased in mothers who give birth post to any natural calamities4.
Children are particularly impacted by the atrocities of climatic alterations5. Overexposure of children to external environment puts them in risk of injury/bites from animals or insects resulting in increased incidence of zoonotic and vector-borne diseases. During the formative phase of children, it is not only physical changes, but also psychological developments occurring in them. Any emotional trauma they suffer during this period, for example, familial loss due to some natural perturbations, can be detrimental for aeons5.
Another vulnerable group is the older population. Most of them would be already suffering from physical and cognitive disabilities or poor mobility and their quick responses to climatic adversities would be impaired6. Majority of them would be dependent on caretakers, a few maybe depending on life-sustaining equipment or certain medications (which has to be refrigerated) and there may not be even power supply in the temporary shelters provided to them6.
The impact of climatic alterations encountered by the LGBT community will be more intense, as they are already deprived of the privileges of a societal inclusion. Most of them are homeless, jobless, and involved in prostitution for a livelihood. This would further escalate during calamities7.
Air Quality
The greenhouse gases emitted from various industries results in air pollution. According to aqi.in data of the year 2022, out of the ten most polluted cities in the world, seven belongs to India of which Delhi is the topmost in India and the second highest in world8. Air pollution in Delhi worsens during the winter season, i.e. from November-February as thick smog is formed due to the combination of winter fog and smoke. The Air Quality Index (AQI) of Delhi in January 2022 was 279, which spiked to 311 in January 20239. Turning towards Kashgar in China, the most polluted city in the world, currently the AQI level is 43610 and it is 187 in Lahore, Pakistan11 which is the seventh most polluted city in the world. The increase of AQI in Delhi during the winter season is concurrently seen with a surge in respiratory illness12.
The following figure depicts air pollution levels worldwide.
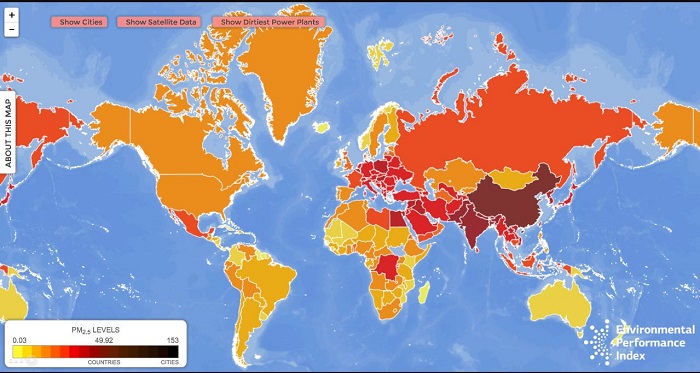
Figure 2: Air pollution levels13 as depicted in the article “Air quality index world map” - Bing (2017). Available at: [http://bit.ly/3FOnNh6]
Recently at Kochi, a city in India, fire broke out at Brahmapuram, a local waste management plant. The smoke was controlled only almost a week later and schools were closed down during the period14. A similar event had taken place at the same location in 2021.
It is a threat to human health as cardiopulmonary diseases are increasingly seen in people inspiring the air containing more particulate matter. In India, the average level of PM2.5 escalated from 60 μg/m3 in 1990 to 76 μg/m3 in 20154. In association with this, deaths due to air pollution surged by 150%, indicating increased health burden and healthcare utilization4.
Socio-culturally, most Indian women are homemakers. They utilize fossil fuel for cooking; hence more exposed to the air pollution occurring within their homes. Consequently, they’re more susceptible to respiratory illnesses. This combines the demographic vulnerability of climate change with the nuisance of air pollution.
Health services
The repercussions of natural calamities on health services are never to be ignored. The term health services encompass hospitals, pharmaceuticals, medical devices, e-health, medical tourism, and medical insurance etc15.
In India, the public healthcare system provides only primary healthcare facilities in most of the villages and urban areas. However, majority of secondary and tertiary healthcare institutions in major cities are owned by the private sector15. Subsequently, there is a markedly skewed distribution of manpower, whereby only 3% of doctors live in rural areas where 70% of India’s population is concentrated16. 1:1000 is the doctor-patient ratio stipulated by the WHO; however, in India it is 1:145616.
Moreover, government expenditure on health in India is 17.3%, while that of China, Sri Lanka and USA are 24.9, 45.4 and 44.1% respectively17. This means the quality of health services in remote and difficult terrains of the country are deficient and substandard17. When natural calamity strikes, this crumbling health system comes to a standstill18. Due to the already disproportionate distribution of medical services and personnel added to power outages, lack of transportation or even the collapse of existing hospitals during disasters, there is upsurge of mortality and morbidity19. Consequent to the destruction of some health facilities, there would be overcrowding in others, which critically diminishes the quality of health care services delivered as witnessed in the US after hurricane Sandy, in Nepal, in Bangladesh (19-21) and elsewhere.
Zoonosis and Climate Change
Zoonotic diseases are classical examples of how environmental changes lead to human illness. Human exploitation of natural resources leads to global warming and habitat destruction, resulting in irreversible changes in ecosystems; consequently, innumerable microbes are spilled from animal kingdom to humans22. While zoonotic diseases like Bubonic plague or Rabies are nothing new to mankind, the rate of transmission of new pathogens (including Covid) has been accelerated massively in recent times due to climatic factors.
Ecosystem fragmentation caused by human activities like agriculture and mining causes loss of biodiversity and this in turn, leads to loss of the dilution effect which reduces the spread of pathogens23. The Ebola virus epidemic in West Africa was a stark example of how deforestation and land shifts may lead to emergence of deadly pathogens. Climate change is also leading to greater geographical range of some hitherto local zoonotic diseases22. Examples include Leishmaniasis in Brazil and Japanese Encephalitis or West Nile Virus in India.
It is estimated that there are thousands of viral species which are potentially harmful to human beings but which are now lying dormant in various animals24. However, due to climate changes and animal poaching, the scope of human-animal contact increases especially for the geographically isolated species, which may provide opportunities for the novel pathogens to give rise to human epidemics. A statistical model has projected that if the current rate of environmental change continues, by 2070, the chance of cross-species transmission in certain biodiversity hotspots of Asia and Africa may be escalated 4000 times24.
LMICs like India are particularly at risk of emerging zoonoses due to high population density and a climate suitable for pathogen spread. In recent years, India has seen repeated outbreaks of zoonoses like Nipah Virus, Kyasanur Forest Disease and Scrub Typhus. Diseases like Zika which was obscured in some countries has now become a global threat. Developing countries like India and Brazil are losing forest covers at an alarming rate25. This, coupled with frequent forest fires caused by climate change, leads to rapid spread of pathogens. Moreover, conditions like temperature and humidity determine the duration of viability of pathogens and with climate change, these factors are also altered favorably for the microbes.
Host factors are also changed due to climatic variations leading to greater transmission of infectious diseases. For example, when humans are exposed to unusual weather conditions; as seen during the recent heat wave in Europe, their level of immunity may decrease which increases the risk of acquiring various infections.
In view of this emerging health threat, urgent action is needed. Increased surveillance and containment efforts are required to limit damages caused by emerging zoonoses. Alternatively, preventive efforts to minimize wild animal-human contact and ensuring safe handling of animals for industrial purposes are also essential26.
Respiratory illness
Amongst multitude of health problems caused by climate changes, the most impacted is the respiratory system. The diseases showing exponential increase are Bronchial Asthma, COPD, rhinosinusitis and various respiratory infections27. People with pre-existing comorbidities like diabetes or bronchiectasis are more affected by climate induced illnesses.
Escalation of respiratory diseases occurs by two mechanisms: firstly, it aggravates conditions like asthma; secondly, it increases exposure to risk factors27. One of the main risk factors for respiratory complaints are pollen. The survival, annual flowering cycle and pollination of vegetation all undergo dramatic changes due to increased frequency of heat waves or precipitation28. Consequent to global warming, many plants show quicker growth, earlier pollen production and longer pollen seasons29. It has been also noted that both the amount of pollen and the amount of allergenic proteins in it are getting higher with time29.
Not only pollens, but fungal spores are also increasing with higher levels of carbon dioxide in the air. Floods are increasing in frequency and the annual number of major floods in Europe is estimated to be doubled by 205027. Frequent flooding leads to more mould formation and hence more fungal spores suspended in the air.
Loss of tree cover enhances air pollution30 leading to respiratory illnesses. The stress, anxiety and/or depression following natural catastrophes like cyclones also act as trigger for asthma31.
The air quality generally gets worsened especially in the cities with climate changes27. Airborne particulate matter is a health hazard and the WHO states that no level of this pollutant could be considered safe for humans27. In many cases, these particulate matter combine with pollens to cause greater harm. After winter season, many cities in Northern part of India are overcast with dense smoke produced by illegal burning of stubbles in the nearby fields. This explosive rise in particulate matter causes epidemics of acute wheezing, coughing and choking amongst city dwellers.
While meteorological events are beyond human control, there are umpteen measures that can be administered to minimize respiratory illnesses. To begin with, early diagnosis of asthmatic diseases especially in children, and early initiation of treatment with steroid inhalers are required. For effective implementation, proper training of medical personnel is also needed. Secondly, environmental engineering can reduce the harms of climate change. This includes discarding fossil fuel usage for cooking and planting non-allergenic trees in densely populated locale.
The management of health system in the face of climate change
Climate change disrupts the health system operations in many ways. At times, the very maintenance of health systems may be disrupted. In Assam, India floods may inundate hospitals in the Brahmaputra valley compelling hospitals to administer even critical drugs like chemotherapy outside, on the road32!
Furthermore, the health systems supply chain may be interrupted by these disasters. One glaring example was Hurricane Maria in Puerto Rico in 201733 which not only jeopardized the health system locally but also affected the health system of entire USA. Puerto Rico is the main manufacturer of IV fluid bags and there was sudden shortage of IV bags all over the country.
However, it should never be ignored that health systems are one of the largest emitters of greenhouse gases. In the USA, healthcare system is responsible for around 9% of total greenhouse gas emissions34. Hence, while health systems must be made more resilient to face the ravages of climate changes, their own carbon footprint should also be reduced. The health systems resilience can be escalated by building climate appropriate infrastructure, like the boat hospitals in Amazon River.
CONCLUSION
Climate change is an imminent threat faced by humanity. All aspects of human society, including the health sector, will be severely impacted by this catastrophe. Inequalities and flaws currently existing in health delivery will be further accentuated by natural disasters. Hence, there is need for urgent policy decisions and coordinated executions to overcome the challenges and to ensure equity.
References:
1. United Nations (no date) What Is Climate Change? | United Nations. Available at: https://www.un.org/en/climatechange/what-is-climate-change.
2. World Health Organization: WHO (2021) Climate change and health. Available at: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health.
3. Dunne, D. (2022) Mapped: How climate change disproportionately affects women’s health. Available at: https://www.carbonbrief.org/mapped-how-climate-change-disproportionately-affects-womens-health/.
4. Sorensen, C. et al. (2018) “Climate Change and Women’s Health: Impacts and Opportunities in India,” Geohealth, 2(10), pp. 283–297. Available at: https://doi.org/10.1029/2018gh000163.
5. Climate Change and Children’s Health | US EPA (2022). Available at: http://bit.ly/3JNQnk0
6. The National Council on Aging (no date). Available at: https://www.ncoa.org/article/climate-change-and-older-adults-planning-ahead-to-protect-your-health.
7. How climate change is affecting the LGBTQIA+ community (no date). Available at: https://www.downtoearth.org.in/blog/environment/how-climate-change-is-affecting-the-lgbtqia-community-74988.
8. Kumar, M. (2023) Top 10 Most Polluted Cities in the World (2022 Data). Available at: https://www.aqi.in/blog/top10-most-polluted-cities-in-the-world/.
9. Kumar, N. (2023) “No ‘good’ days for Delhi air in Jan as winter makes pollution worse,” www.business-standard.com, 3 February. Available at: https://www.business-standard.com/article/current-affairs/aqi-above-moderate-levels-for-29-days-in-january-no-good-day-since-2016-123020301223_1.html.
10. AQI (no date) “Kashgar Air Quality Index (AQI) : Real-Time Air Pollution | Xinjiang,” AQI. Available at: https://www.aqi.in/us/dashboard/China/xinjiang/Kashgar.
11. The World Air Quality Index project (no date) “Lahore Air Pollution: Real-time Air Quality Index,” aqicn.org. Available at: https://aqicn.org/city/lahore/.
12. Upadhyay, A. (2023) “Delhi’s OPDs report spike in respiratory complaints amid chill, pollution,” The Indian Express, 11 January. Available at: https://indianexpress.com/article/cities/delhi/delhis-opds-report-spike-in-respiratory-complaints-amid-chill-pollution-8374183/.
13. Air quality index world map - Bing (2017). Available at: http://bit.ly/3FOnNh6
14. BBC News (2023) Brahmapuram fire: India’s Kochi city covered in toxic haze from waste dump fire. Available at: https://www.bbc.com/news/world-asia-india-64835273.
15. India Brand Equity Foundation (no date) “Healthcare System in India, Healthcare India - IBEF.” Available at: https://www.ibef.org/industry/healthcare-india.
16. Addressing the challenges of the Indian healthcare system - Opinions - Tata Trusts (no date). Available at: https://www.tatatrusts.org/insights/opinions/addressing-the-challenges-of-the-indian-healthcare-system.
17. Mehta, P. (2015) 7 Major Problems of Health Services in India. Available at: https://www.economicsdiscussion.net/articles/7-major-problems-of-health-services-in-india/2305.
18. Santalahti, M., Sumit, K. and Perkiö, M. (2020) “Barriers to accessing health care services: a qualitative study of migrant construction workers in a southwestern Indian city,” BMC Health Services Research, 20(1). Available at: https://doi.org/10.1186/s12913-020-05482-1.
19. “The Impact of Climate Change on Our Health and Health Systems” (2022) Commonwealth Fund [Preprint]. Available at: https://doi.org/10.26099/49re-ky81.
20. Karn, M. and Sharma, M. (2021) “Climate change, natural calamities and the triple burden of disease,” Nature Climate Change, 11(10), pp. 796–797. Available at: https://doi.org/10.1038/s41558-021-01164-w.
21. Chowdhury, N.I. (2022) “Right to Health in Bangladesh in the Situation of Post Natural Calamities: An Analytical Overview,” Social Science Research Network [Preprint]. Available at: https://doi.org/10.2139/ssrn.4261146.
22. Twin threats: climate change and zoonoses (Editorial). The Lancet Infectious Diseases 2023; 23: 1. doi: https://doi.org/10.1016/S1473-3099(22)00817-9
23. WHO. New report highlights the impact of changes in environment on One Health. [2022 Jul 1; Cited 2023 Mar 19]. Available online from https://www.who.int/europe/news/item/01-07-2022-new-report-highlights-the-impact-of-changes-in-environment-on-one-health#:~:text=Climate%20change%20and%20rising%20temperatures,of%20both%20pathogens%20and%20vectors.
24. Carlson CJ, Albery GF, Merow C et al. Climate change increases cross-species viral transmission risk. Nature 2022; 607: 555-62
25. Kumari R, Banerjee A, Kumar R et al. Deforestation in India: Consequences and Sustainable Solutions. [Open access chapter IntechOpen]. DOI: 10.5772/intechopen.85804
26. Tiwari Dhiman R. Emergence of zoonotic diseases in India: A systematic review. Med Rep Case Stud. 2018;3:163–70
27. D’Amato G, Cecchi L, D’Amato M et al. Climate change and respiratory diseases. European Respiratory Review 2014; 23: 161-169
28. Hegerl GC, Zwiers FW, Braconnot P, et al. Understanding and attributing climate change. In: Intergovernmental Panel on Climate Change. Climate Change 2007 – The Physical Science Basis: Working Group I Contribution to the Fourth Assessment Report of the IPCC. Cambridge, Cambridge University Press, 2007; pp. 663–746
29. Pielke RA, Cecchi L, D’Amato G, Annesi-Maesano I. Climate, urban air pollution and respiratory allergy. In: Pielke RA , ed. Climate Vunerability: Understanding and Addressing Threats to Essential Resources. Waltham, Academic Press, 2013; pp. 105–113
30. Schiermeier Q. Climate and weather: extreme measures. Nature 2011; 477: 148–149
31. Kar N, Mohapatra PK, Nayak KC, et al. Post-traumatic stress disorder in children and adolescents one year after a super-cyclone in Orissa, India: exploring cross-cultural validity and vulnerability factors. BMC Psychiatry 2007; 7: 8
32. Assam Floods: How this cancer hospital is treating patients. LiveMint. [Published 2022 Jun 28; Cited 2023 Mar 20]. Available online from https://www.livemint.com/news/india/assam-floods-how-this-cancer-hospital-is-treating-patients-11656410228224.html
33. Chen A, Murthy V. How Health Systems Are Meeting the Challenge of Climate Change. Harvard Business Review, 2019. Available online from https://hbr.org/2019/09/how-health-systems-are-meeting-the-challenge-of-climate-change
34. Shanoor Seervai, Lovisa Gustafsson, and Melinda K. Abrams, “How the U.S. Health Care System Contributes to Climate Change,” explainer, Commonwealth Fund, Apr. 2022. https://doi.org/10.26099/m2nn-gh13