Ultrasound equipment has become more affordable and portable over the last decade as its use has become commonplace outside of the radiology suite. Recent studies have shown that with minimal training and augmented protocols, sonography can improve resuscitative efforts outside the hospital in prehospital care.
Introduction
Bedside point of care ultrasound (POCUS) has rapidly become a critical tool for emergency medicine providers in the emergency department to aid in diagnosis and procedures, particularly to guide resuscitative efforts and identifying so-call “reversible causes” in cardiac arrest and other situations calling for cardiopulmonary resuscitation (CPR). One of the main drivers of this trend has been technology advances allowing ultrasound machines to be smaller, lighter, easier to use, and more affordable for emergency departments to purchase.
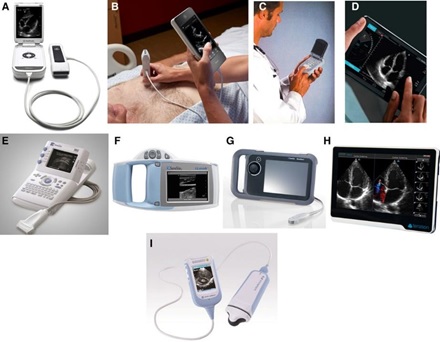
Figure 1: Mohammed A. Chamsi-Pasha. Circulation. Handheld Echocardiography, Volume: 136, Issue: 22, Pages: 2178-21881
Given its proven value in CPR and in trauma, it should come as no surprise that recent studies have explored the utility of these newer, portable ultrasound machines in the pre-hospital setting assessing whether the use of ultrasonography medicine service (EMS) providers with critically ill patients could help direct the efforts of emergency. Over the last several decades, technologies previously found only in hospitals or emergency departments have similarly become more portable and able to be brought into the field and on the ambulance by EMS. Some examples of this include portable electrocardiogram (ECG) machines and automated defibrillators to diagnose and treat heart arrhythmias. Portable pulse oximeters and carbon dioxide detectors have also been incorporated into these units to give real-time information about a patient’s respiratory state.

Figure 2: Biphasic defibrillator, ECG, NIBP SpO2 monitor from: https://commons.wikimedia.org/wiki/File:Biphasischer_Defibrillator.jpg
A potential argument against the use of ultrasonography by emergency medicine technicians (EMTs) and paramedics is that they do not have the training or skill to safely use and interpret the ultrasound images, but the same was likely said about paramedics interpreting ECGs independently and was the argument against anyone other than radiologist reading ultrasounds that has been debunked by the wide-spread safe use by physicians and advanced practice providers.
Currently, ECG, pulse oximetry, and capnography are indispensable and integral in resuscitation according to the Advanced Cardiac Life Support (ACLS) guidelines.2 Similarly, POCUS has been shown to be invaluable in the rapid assessment of trauma patients and has been incorporated into certification in Advanced Trauma Life Support (ATLS).1 In pre-hospital care, EMTs and paramedics are taught and follow ACLS and other algorithms with specific interventions according to the diagnosed cause of cardiac arrest or arrhythmia. Portable ECG, pulse oximetry, and capnography allow EMS providers to identify and thus treat life threatening conditions earlier. Portable ultrasound, if employed judiciously, can have the same effect and positive impact on pre-hospital care.
Pre-hospital Application of POCUS
The pre-hospital setting has unique challenges in an ever changing, noisy, and chaotic environment. One of the strengths of ultrasound is that it can provide visual information that can be seen and captured at relatively low cost, outside the hospital. If applied in the appropriate circumstances with the right patient, an adequately trained professional ultrasonography can aid in diagnosis and treatment in the pre-hospital setting. Several studies3 have proposed algorithms for the use of ultrasound in the prehospital setting already, and some algorithms currently implemented within the hospital (Table 1). ATLS which advocates for the use of ultrasound in the Extended Focused Use of Sonography in Trauma (EFAST) which looks for evidence of blood in the abdomen or thorax or a collapsed lung, could potentially be transferred to the field.
| Protocol | Study | Application | Pertinent Findings |
| FEEL | Focused Echocardiographic Evaluation in Life support | Identify reversible causes* during CPR in cardiac arrest | Pericardial effusion, right heart strain, LV dysfunction, collapsing IVC, fine VF |
| US-CAB | Ultrasound protocol for Circulation-Airway-Breathing | Sequential evaluation of circulation (heart and IVC), airway (trachea), and breathing (lungs) | Pericardial tamponade, collapsing IVC, esophageal intubation, lack of lung slide |
| CASA | Cardiac Arrest Sonographic Assessment (CASA) exam – A standardized approach to the use of ultrasound in PEA | Three, < 10 second POCUS exams that occur at pulse checks during CPR to identify reversible causes* of PEA | Cardiac tamponade, right heart strain, cardiac activity |
| PAUSE | Prehospital Assessment with UltraSound for Emergencies (PAUSE) protocol. | Pleura exam followed by focused TTE (subxiphoid, parasternal long views) | Assessment for pericardial effusion, pneumothorax, and the presence/absence of cardiac activity |
Table 1: Summary of pre-hospital protocols integrating POCUS.3-8 *Reversible causes = Pericardial tamponade, tension pneumothorax, pulmonary embolism, hypovolemia. CPR = cardiopulmonary resuscitation, LV = left ventricle, IVC = inferior vena cava, VF = ventricular fibrillation, PEA = pulseless electrical activity, TTE = transthoracic echocardiogram

Figure 3: Paramedics using ultrasound during CPR with mechanical compressions from: Point-of-Care Ultrasound in the Prehospital Setting4
The A-B-Cs of Pre-Hospital Ultrasound
Outside of protocols, there are other ways that POCUS has been successfully used in the hospital and can be employed in the pre-hospital setting to identify potential life-threats and other emergencies quickly, efficiently, and accurately. This is similar to the use of a stethoscope or palpation that EMS providers already use regularly to check for pulses or listen for breath sounds. In some of these procedures and potential uses, ultrasound can be more accurate than auscultation or palpation.
A commonly used acronym for the first steps in assessment of a potentially critically ill patient is to check the “A, B, C's” which means assessing the patient’s Airway, Breathing, and Circulation. These are universal emergency medicine steps that EMS regularly follow in the first few minutes of pre-hospital care of unconscious patients, those in respiratory distress or failure, and patients with potential cardiac arrest or severe cardiac dysfunction. Any of these emergencies require rapid identification and correction on scene and during transport to the hospital for best outcomes.
Each step during the Airway, Breathing, and Circulation assessment and treatment of critically ill patients can be enhanced by the use of ultrasound if properly trained and executed by EMS. The following is a summary of the potential uses of POCUS in the unconscious patient or those in respiratory or cardiovascular failure:
● Airway – POCUS can identify an endotracheal tube in the esophagus.
● Breathing – POCUS can assess for lung sliding, the absence of which can indicate a pneumothorax and help decision making to perform needle decompression.
● Circulation – Ultrasound can quickly and accurately check pulses and cardiac motion guiding the need for chest compressions.
The best, fastest, and most logical use of pre-hospital ultrasonography lies in asking binary questions where a rapid evaluation with ultrasound can answer yes or no, with operators discontinuing the use of POCUS if definitive images cannot be obtained due to body habitus, machine, or user limitation and especially in cases where the operator does not have the training or expertise to interpret the images.
Limitations of Pre-hospital Sonography
Both studies and protocols above included an additional person operating and interpreting the ultrasound images which could be quite a shift and salary expense for many EMS systems, although this might be feasible for critical care transport teams such as flight EMS teams. Another cost would be purchasing portable ultrasound machines and training first responders in the appropriate use of the technology. Upkeep, maintenance, and troubleshooting would also add a recurring cost.
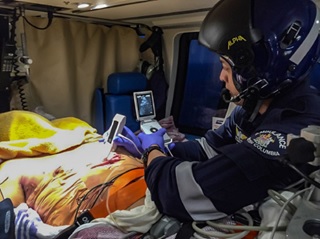
Figure 4: British Columbia Ambulance Service Critical Care Paramedic Using Ultrasound from: A Blended Prehospital Ultrasound Curriculum for Critical Care Paramedics5
The biggest danger in introducing ultrasound to the pre-hospital setting would be the inappropriate use of ultrasound that delays critical interventions as seen in studies showing in-hospital delays during pulse checks longer than 10 seconds during CPR6,7 or also the inaccurate utilization resulting in an unnecessary or harmful intervention.7
The future of POCUS in the field
The use of POCUS in the hospital has expanded dramatically over the last decade proving to be safe, valuable, and rapid in diagnosis, and has become standard of care for visualizing subcutaneous structures during procedures such as placing central intravenous catheters. With the portability of ultrasound machines now the size of a smartphone or tablet, and the cost no longer prohibitive, it is without doubt that the next ten years will see a rapid rise in the use of pre-hospital POCUS by paramedics and other physician extenders. The key remains incorporating POCUS into proven pre-hospital protocols in a way that does not delay essential care. It is likely that more studies will show that this is feasible and improves outcomes. Further demonstration that the core skills of POCUS can be taught in EMS training efficiently without adding an excessive or prohibitive number of hours will be needed for approval and implementation within long-standing, widely used protocols.
Ultrasound is best used in the prehospital setting in scenarios where an ultrasound finding would enhance pre-hospital care. This would include the use of sonography to answer binary questions discussed in detail at the end of the chapter. Delaying care to perform an ultrasound or focusing on irrelevant findings are potential risks to its pre-hospital application. Using the Airway, Breathing, Circulation (A-B-C) approach to the critically ill or injured patient, important findings that are pertinent to the pre-hospital care, can be quickly and easily answered with sonography if there is no delay in treatment.
At this juncture in time, it is not a matter of if ultrasound will be used by EMS, but how it will be employed. Already there are cautionary studies showing detrimental results when attempts to ultrasound delay critical care interventions such as chest compression. Prudent early adopters should focus on a narrow scope of indications with easy to interpret ultrasound findings that lead to immediate change in treatment of life threats rather than opening Pandora’s box and likely wasting time and resources to needlessly “look around” with the ultrasound rather than providing good, timely pre-hospital critical care.
References:
1. Chamsi-Pasha MA, Sengupta PP, Zoghbi WA. Handheld echocardiography: Current state and future perspectives. Circulation. 2017;136(22):2178-2188. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.117.026622?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed. Accessed Mar 14, 2023. doi: 10.1161/CIRCULATIONAHA.117.026622.
2. Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: Adult basic and advanced life support: 2020 american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142(16_suppl_2):S366-S468. Accessed Mar 14, 2023. doi: 10.1161/CIR.0000000000000916.
3. Lien W, Hsu S, Chong K, et al. US-CAB protocol for ultrasonographic evaluation during cardiopulmonary resuscitation: Validation and potential impact. Resuscitation. 2018;127:125-131. https://www.sciencedirect.com/science/article/pii/S0300957218300613. Accessed Apr 2, 2022. doi: 10.1016/j.resuscitation.2018.01.051.
4. MD FHA. Point-of-care ultrasound in the prehospital setting. . 2018. https://www.jems.com/patient-care/point-of-care-ultrasound-in-the-prehospital-setting/. Accessed Mar 15, 2023.
5. Guy A, Bryson A, Wheeler S, McLean N, Kanji HD. A blended prehospital ultrasound curriculum for critical care paramedics. Air Med J. 2019;38(6):426-430. Accessed Mar 15, 2023. doi: 10.1016/j.amj.2019.07.013.
6. Huis in 't Veld, Maite A., Allison MG, Bostick DS, et al. Ultrasound use during cardiopulmonary resuscitation is associated with delays in chest compressions. Resuscitation. 2017;119:95-98. https://www.sciencedirect.com/science/article/pii/S0300957217303027. Accessed Feb 22, 2022. doi: 10.1016/j.resuscitation.2017.07.021.
7. Veld, Maite A. Huis in 't, Allison MG, Bostick DS, et al. Ultrasound use during cardiopulmonary resuscitation is associated with delays in chest compressions. Resuscitation. 2017;119:95-98. https://www.resuscitationjournal.com/article/S0300-9572(17)30302-7/abstract. Accessed Feb 12, 2022. doi: 10.1016/j.resuscitation.2017.07.021.