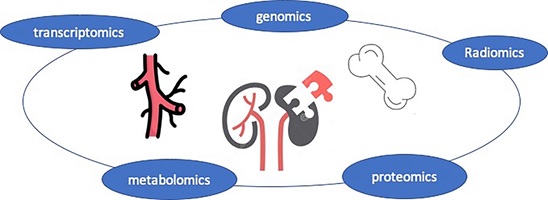
The evolving therapies to treat the complications and replace kidney, although having prolonged the life span of patients with chronic kidney disease (CKD), still leave critical issues (e.g. cardiovascular risks). The ‘omics’ techniques (e.g. genomics, proteomics, metabolomics, and transcriptomics) are “molecular glasses” which lead us to the full bloom of precision medicine.
Challenges in CKD-MBD
Chronic kidney disease (CKD) is caused by a range of pathogenesis and becoming the leading burden of mortality and morbidity in the world. It is assumed that CKD will become the 5th most common cause of death worldwide in 2040. Despite the big leaps made in the last decades, we are still facing a lot of unmet needs. For instance, we still do not have specialized target lab values among different age, gender, and race. In addition, no approved or well-tested treatment has been discovered to retard the progress of vascular calcification and promote the survival rate. On the basis of renal replacement techniques development, how to balance the life quality and the excessive intake of minerals is still a huge problem. Furthermore, we need to know how to deal with aging, inflammation, and nutrition deficiency to improve the outcomes of CKD patients.
Among all these problems, chronic kidney disease-mineral and bone disorders (CKD-MBD) has long been discussed but difficult to address. Cardiovascular events due to vascular calcification and fracture due to osteoporosis are two main reasons that lead to low quality of life and death.
Precision medicine is a broad and obscure concept which came following the rise of gene engineering. Different from personalized medicine, precision medicine put more emphasis on identification of clinical patterns using advanced technologies. Such diagnostic strategies and targeted treatments requires a deep understanding of disease biology and the ability to dissect the relationship between molecular and genetic factors and their phenotypic consequences. As the “omics” techniques keep developing, we are gaining new tools that are powerful to help us understand more essential pathogenesis and seek more precise therapies of CKD-MBD.
Metabolomics
Methods for metabolomics mainly include nuclear magnetic resonance (NMR), mass spectrometry (MS), and metabolic flux analysis (MFA). These methods can be adopted alone or in combination to the others to identify and quantify a wide range of metabolites. MS can be coupled with other analytical techniques and further classified into ion mobility-MS (IM-MS), direct injection-MS (DI-MS), liquid chromatography-MS (LC–MS), capillary electrophoresis-MS (CE-MS) and gas chromatography-MS (GC–MS).
Metabolomics techniques have been used in the prediction or diagnosis of special clinical pattern of CKD-MBD. For instance, difference in metabolites can reflect difference in bone metabolism in CKD patients. A range of metabolites involved in protein synthesis, amino acid, energy, steroid hormone have been discovered to be associated with elevated iPTH in patients with end-stage renal disease (ESRD) using LC-MS metabolic prefiling. Bone biopsy is the gold standard for diagnosis of different osteodystrophy. However, metabolites screened using NMR combining with demographical information may be comparable in their values to diagnose bone disease as bone biopsy. ethanol was associated with mineralization disorder, and low carnitine was seen in patients with low bone Dimethylsulfone, glycine, citrate, and N-acetylornithine could indicate bone turnover, low volume.1 Of note, L- carnitine has been widely used in hemodialysis patients as a beneficial supplement which has proved to significantly reduces oxidative and inflammatory stress, erythropoietin-resistant anemia, and comorbidities such as tiredness, impaired cognition, muscle weakness, myalgia, and muscle wasting. Whether it can be a target to treat osteodystrophy in CKD needs further investigation. The relationship between microbiomes and CKD has been hotspot for research for several years. Metabolomics indicate that gut microbiomes and its metabolites can regulate the bone metabolism by interacting with immune cells.2 The role of treating or modifying microbiomes in dealing with CKD-MBD are warranted in the future.
Proteomics
As the technique evolves, we are entering an era with more accurate multilevel proteomics testing. Based on the hierarchy of the aimed proteins, proteomics could be classified into three categories: bottom-up proteomics, top-down proteomics, and native proteomics. Integration of deep learning into proteomics profiling and analysis help make breakthroughs in techniques.
Several signal pathways (e.g. Wnt signaling, TGF- β, RANKL) play important roles in CKD-MBD. Using proteomics, proteins in different tissues or organs could be screened and linked with bone metabolism parameters. Denosumab targeting RANKL has been used in CKD patients with osteoporosis pushing us one more step to impede the progression of renal osteopathy. However, no single pathway can explain the whole view. We need to launch more studies integrating the information regarding interactions among inflammation, bone metabolism, and coagulation and anticoagulation system.
Genomics
With the development of large scale GWAS, many genetic signals associated with renal osteodystrophy and related traits have since been reported. However, identifying underlying gene responsible for these genetic associations, a prerequisite for drug targets, remains a challenge. "Osteocyte signature" has been entitled following the development of bone phenotyping and functional study models (e.g. knockout mice and zebrafish) to describe the facilitated characterization of bone disease provided by genomics. Based on the expanding "multi-omics" database resources, potential molecular mediators such as mRNA expression, protein expression, and DNA methylation levels leading to the discovery of signal pathways are studied.
Genome-wide association studies (GWAS) prompt understanding of the genetic determinants of circulating levels of 25-hydroxyvitamin D, calcium, phosphorus, fibroblast growth factor-23, parathyroid hormone, fetuin-A and osteoprotegerin. However, what remain to be answer are how kidney function impacts these processes and which biomarker, and whether certain genetic variant casts impact on kidney structure and functions. Mendelian randomization, known as a perfect instrumental variable, may help answer the questions.
Transcriptomics
Transcriptomic analyses are promising in detecting intrinsic modifications within different cells located in bone and vessels. Major techniques including bulk RNA sequencing (RNAseq) and single cell RNAseq (scRNAseq), represent a possible solution to the complexity of CKD-MBD by using molecular expression profiles to determine the underlying cell and molecular mechanisms. Compared to RNAseq, scRNAseq is more cost-effective and allows the detection of the most represented transcripts corresponding to large variations in gene expression in distinct cell populations, but it may not be as sensitive at detecting changes.3 Nowadays, transcriptomics has been adopted to sense the changes during the progression of CKD-MBD complications and correspondent to candidate treatments. Single cell manner detection using scRNAseq might provide more assistance for us to understand the complexity of vascular calcification and renal osteodystrophy in CKD patients.
Radiomics
Radiomics is a newly emerging concept of integrating deep learning to analyze a large amount of quantitative features from medical images for imaging biomarker discovery and validation for different diseases. Regarding CKD-MBD, machine learning helps us to analyze calcification in vessels and tissues multifacetedly which allows using different parameters to assess the calcification and predict the prognosis. In addition, radiomics might help reflect information beyond bone mineral density allowing us to recognize different patterns of osteodystrophy noninvasively. The progress of radiomics will provide us more abundant radiological features assisting diagnosis, supervision of drugs, and outcome prediction. Additionally, radiomics provide opportunities to interpret multiple clinical topics in single examination. For instance, by using deep learning in low-dose CT (LDCT) can offer a “one-stop” test for both lung cancer screening and cardiovascular risk stratification in at-risk subjects including CKD patients.
The future of precision medicine in “omics” era
Of note, single cell “omics”, “multi-omics”, and machine learning-aided “omics” are on the rise. In the center of a world with information explosion, the aim of “omics” we conduct should be clearer. Linking “omics” with precision medicine, we are able to sense or detect more subtle changes and bridge them with clinical significance. Future perspectives lie in multiple aspects. First, integration of different “omics” will make the medicine specialized for different individuals not only from clinical presentation, but from multifaceted “omics” presentation (e.g. genes, proteins, metabolites, and radiology). Secondly, “multi-omics” and machine learning are participating in every phases of drug development to help design new therapies. Landmark therapies are expected to reverse the progression of CKD-MBD, thus prolong the life span of CKD patients. Furthermore, rapid and noninvasive determination of clinical pattern is not a dream, with artificial intelligence-aided decision making and comprehensive analysis of the substitutes and images provided by “omics”.
References
1. Baptista AL, Padilha K, Malagrino PA, et al. Potential Biomarkers of the Turnover, Mineralization, and Volume Classification: Results Using NMR Metabolomics in Hemodialysis Patients. JBMR Plus. Jul 2020;4(7):e10372. doi:10.1002/jbm4.10372
2. Kermgard E, Chawla NK, Wesseling-Perry K. Gut microbiome, parathyroid hormone, and bone. Curr Opin Nephrol Hypertens. Jul 1 2021;30(4):418-423. doi:10.1097/MNH.0000000000000714
3. Martin A, David V. Transcriptomics: a Solution for Renal Osteodystrophy? Curr Osteoporos Rep. Jun 2020;18(3):254-261. doi:10.1007/s11914-020-00583-6