Southeast Asia’s healthcare access ecosystem is now at a critical juncture. To improve access for the long term, Joseph shares why healthcare stakeholders in the public and private sectors must enhance sustainability around the key aspects of finance, treatment and health systems.

Southeast Asia's healthcare landscape has irrevocably changed. Due to the demographic shifts the region has been experiencing such as ageing populations1 and the rise in non-communicable diseases (NCDs)2 governments and healthcare stakeholders must now reassess3 healthcare expenditure and reforms to not only improve health ecosystems in terms of equitable access, but also sustainability.
However, a major challenge to these is that the healthcare ecosystem has not evolved in tandem with broader socio-economic development4, especially in Southeast Asia's emerging markets. This challenge was exacerbated further due to COVID-19, which spotlighted the gaps5 within the region's healthcare access ecosystem.
Southeast Asia's healthcare access ecosystem is now at a critical juncture. To improve access for the long term, healthcare stakeholders both in the public and private sectors must focus on enhancing sustainability around the key aspects of finance, treatment and health systems. Achieving this requires placing patient-centricity at the core, namely by striving to achieve better health outcomes for them.
Generating better outcomes for patients requires supporting them throughout their treatment journey even at the very beginning. This can be done by ensuring that access needs to be a core component of every pharmaceutical company's overall strategy. It is a crucial step before implementing any access solution; it must be considered during the planning process and not just as an afterthought.
Providers need to deploy more patient-centric approaches that involve patients throughout their healthcare journey. This can be done by ensuring those solutions are specifically tailored to them and consider them as individuals, as access is being redefined from a short-term, one-off strategy to a long-term solution.
To do so, patient-based solutions must focus on the entire patient journey, starting with access to diagnosis. Before being able to access6 treatment, many patients face a long process to get referred to the right specialist, get misdiagnosed or cannot afford the diagnostic tests especially for rare diseases. Improving diagnosis access thus requires disease awareness and physician capacity building, in addition to giving patients more financial support to access diagnostic testing.
Additionally, solutions must also consider treatment affordability. Many people in Southeast Asia are particularly vulnerable in terms of healthcare financing7 and governments have been working on health financing reforms8 to reduce dependence on out-of-pocket payments. As much as these efforts are important and significant, they are not sufficient to cater for all health care needs. The private sector can play a supportive role here via cost-sharing programmes9 and tools that measure patients' financial capabilities10 to help determine how much monetary assistance patients need to follow through on their treatment in the long term.
Healthcare ecosystem stakeholders can also offer services to support patients throughout their treatment journey to ensure patients receive the full course of treatment and maximise treatment benefits. This is as non-adherence rates are rising across the region, even in more mature markets like Singapore11 and Malaysia12. If left unchecked, the long-term effectiveness of treatments would be compromised and may critically affect a population's overall quality of life. Better health outcomes for patients can be achieved by making adherence interventions more effective, as studies13 note that doing so can potentially generate more impact on a patient's health more so than making improvements in specific treatments. This is as medical advances would inevitably face obstacles in fulfilling their potential to reduce illness burdens, especially for chronic cases, if a system that addresses adherence determinants does not exist. Essentially, treating diseases successfully requires doing more than just improving access to medications. This is why interventions are essential. A multi-sectoral approach will help improve medical outcomes by making it easy for patients to track and manage their treatment via Patient Support Programs (PSPs).
Another focal point is ensuring robust compliance with access initiatives. Unsafe medical care contributes to poor patient outcomes, a challenge that is especially pertinent in emerging markets14 within Southeast Asia. Patient access programmes must go beyond being just well-designed. Program management must fully comply with the region's best practices in standard operating procedures (SOPs), data security conformity with General Data Protection Regulation (GDPR) and local data privacy policies in each country, patient consent, and pharmacovigilance15.
Existing healthcare infrastructures, particularly hospitals, are now being stretched to their limits. Simultaneously, populations are growing and healthcare demands are rising pressure points growing even before COVID-19, which has further exacerbated this dire situation16. Hence, the proliferation of digital tools and solutions outside of hospitals (namely, those that can complement existing services) must be raised.
Today, digital healthcare solutions are being promoted in advanced markets like Singapore17 and even in more emerging economies, such as Thailand18, which uses more advanced technologies such as 5G to improve telehealth services. More can be done to stimulate similar advancements but promoting the use of digital tools that can enable effective out-of-hospital services must also be taken on by private sector healthcare ecosystem actors to help reduce patient reliance on in-hospital services. This is a crucial step in building a digital ecosystem that connects different stakeholders in the patient's journey in the programmes they are in including the patient themselves, the physician, the pharmacist, the pharmaceutical companies, civil society groups such as charities, as well as labs and distributors.
When designing digital solutions, patients must remain at the core; patient centricity must be maintained amid the move to making processes faster, simpler and easily accessible for them and to improve engagement between healthcare system stakeholders. This can ultimately lead to an increase in adherence in health programmes.
Diagnosis, access and adherence programmes that are digitally delivered and personalised can also facilitate and expedite the patient journey. While ensuring the human interaction still plays an important part, the greater proliferation of data can help improve decision making and programmes improvements. Real-world insights gleaned from access programmes can help deliver breakthrough insights on disease evolution, treatment, patients' perceptions, outcomes and cost.
The creation of an access ecosystem can generate greater financial, treatment and health system sustainability. Here, multi-sectoral collaboration is crucial in supporting governments that have long been stretched in improving access by themselves.
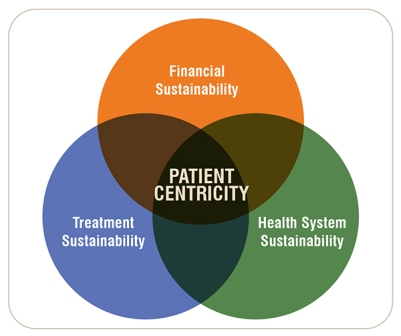
When access initiatives are designed with the patient in mind over the long term, we can attain the following three pillars of healthcare sustainability:
Financial sustainability
By designing initiatives that are personalised to the patient, the financial support provided is no longer limited to budget constraints of the government, pharmaceutical company or the patient. The multistakeholder collaboration allows the initiatives to be financially sustainable and can be scalable over time to reach as many patients as possible, while the patients don't eventually need to pay out-ofpocket amounts that are beyond their means.
Treatment sustainability
By addressing both affordability and adherence challenges, more patients can stay on their prescribed treatment for as long as medically necessary, ensuring they are getting the maximum benefit from their treatment. At the same time, physicians would have a greater capacity to treat more patients.
Health system sustainability
By complementing the healthcare system with patient management mechanisms implemented outside of health institutions (i.e., hospitals), burdens can be lifted from the healthcare system, enabling it to cope with the increasing older population, improves the cost-effectiveness of healthcare interventions, ensuring better health outcomes, and allows the healthcare system to expand, keeping the expenditures in proportion to the GDP sustainable.
When we address access holistically, we achieve this trifecta of sustainable access. We have seen this first-hand in Axios-managed Patient Support Programs. For instance, we collaborated with a multinational pharmaceutical company to develop their 'access to medicine strategy', ensuring that access was not an afterthought. Together we designed a shared payment access programme. The programme is focused on improving access to treatment for selected haematological and gastroenterological conditions. It was important to go beyond just reimbursement and identify a more tailored approach that segments the patient population.
This programme uses Axios' Patient Financial Eligibility Tool (PFET) that considers both formal and informal income sources enabling patients to complete their prescribed treatment even if they can't afford to pay for it in full. By understanding the individual patient's circumstances, we can define a quantity of payment comfortably within their means and ensure that only those who need the support benefit from it. The company was able to reach its average discount goal without reducing the price. At the same time patients only paid what they could afford and so it became financially sustainable.
The cost-sharing has significantly reduced the financial burden, resulting in larger patient enrolment in the programme with more patients able to stay on treatment, which significantly improved the duration of treatment, reaching optimal medical outcomes. In fact, in 75 per cent of cases, a higher-than-expected duration of treatment was reached. Concurrently, this led to broader healthcare provider satisfaction and so enrolment accelerated. Here, treatment sustainability was reached.
The programme was then able to scale globally now supporting patients in Asia, Africa, Europe, Middle East and Latin America. For some countries, our suite of digital tools has connected patients to their healthcare providers outside of the hospital care setting while integrating stakeholder coordination into one seamless ecosystem, which became essential during the pandemic. With many more patients able to access and stay on treatment longer, while having an out-of-hospital support system to complete the HCP efforts, the burden on the healthcare system is lighter, especially as patients adhering to treatment means less complications and less hospitalisations. By doing so, we keep the healthcare system sustainable and ready to extend care to more patients.
Southeast Asia's healthcare access ecosystem is being strained to the point that it cannot quickly adapt to patients' ever-evolving needs. The region's population is growing at a rate of knots, and the increasing population density means the healthcare system cannot rely solely on hospital care anymore; Because hospitals are not equipped to care alone for patients living with lifelong conditions or chronic diseases requiring long-term treatment forever. The patient must return home at some point, so there is a considerable gap in care because HCPs cannot be everywhere. If patients are on treatment that requires technical expertise like a self-administered injection, they need to be supported, or adherence rates will drop, patients will not get the full medical benefits from the treatment, and their condition could worsen. We must build and extend healthcare capabilities beyond the hospital while keeping patients connected to facilitate the patient journey. By conservative estimates, the pandemic has accelerated the digital transformation of healthcare by at least five years, and technology is essential to integrating all components of a multi-faceted ecosystem that reaches patients wherever they are. Patient support programmes include medication management and counselling, significantly improve care and overall patient experience in chronic disease states, especially with complex therapies. The goal is to generate more, improved health outcomes for the region's patients in the long term, supported by a robust network that plays to the strengths of every collaborating stakeholder.
True healthcare access sustainability can be achieved through such outcomes, but a multi-sectoral, multidimensional response must support the process. This call has to be taken actioned by access specialists in both the public and private sectors and by placing patients at the centre of their healthcare access strategies.
References:
1 https://www.who.int/southeastasia/health-topics/ageing
2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7371561/
3 https://www.adb.org/sites/default/files/publication/684701/adbi-wp1220.pdf
4 https://iigh.unu.edu/publications/articles/health-andhealthcare-systems-in-southeast-asia.html
5 https://www.brookings.edu/blog/order-from-chaos/2021/01/14/covid-19-in-southeast-asia-regional-pandemic-preparedness-matters/
6 https://www.who.int/southeastasia/news/detail/04-09-2018-countries-in-who-south-east-asia-regionresolve-to-make-essential-medical-products-accessibleaffordable-to-all
7 https://www.who.int/southeastasia/health-topics/healthfinancing
8 https://www.researchgate.net/publication/49787717_Health-financing_Reforms_in_Southeast_Asia_Challenges_in_Achieving_Universal_Coverage
9 https://axiosint.com/accessinthailand
10 https://www.liebertpub.com/doi/abs/10.1089/pop.2012.0049?journalCode=pop&
11 https://journals.sagepub.com/doi/full/10.1177/2010105820933305
12 https://www.researchgate.net/publication/332804991_Interventions_on_Improving_Medication_Adherence_in_
Malaysia_A_Mini_Review
13 https://pubmed.ncbi.nlm.nih.gov/12076376/
14 https://academic.oup.com/intqhc/article/27/4/240/2357347
15 https://www.who.int/teams/regulation-prequalification/regulation-and-safety/pharmacovigilance
16 https://www.internationalaffairs.org.au/australianoutlook/southeast-asias-responses-to-the-covid-19-pandemic/
17 https://www.edb.gov.sg/en/business-insights/insights/thehealthtech-boom-in-southeast-asia-big-strides-and-newopportunities-for-healthcare.html
18 https://techwireasia.com/2020/12/thailand-aims-to-bethe-new-apac-medical-hub-leveraging-smart-health/