Telemedicine has the potential to provide accessible and equitable healthcare. The use of telemedicine has accelerated after the COVID-19 pandemic, especially in the field of cardiology. Our article explores the applications of telemedicine for patients with heart failure, including remote monitoring and consultation, and the benefits and limitations of telemedicine.

Remote healthcare and telemedicine utilize various information technology to provide healthcare services remotely between a patient and provider when both parties are distant. These services expanded rapidly during the beginning of the COVID–19 pandemic and remain a crucial part of healthcare delivery today. Before March 2020, telemedicine was used periodically, with approximately 76% of the United States hospital healthcare systems employing remote healthcare delivery on a case-by-case basis. Although numerous specialties utilize these modalities, Cardiology, Radiology, and Psychiatry use remote healthcare and telemedicine most frequently.
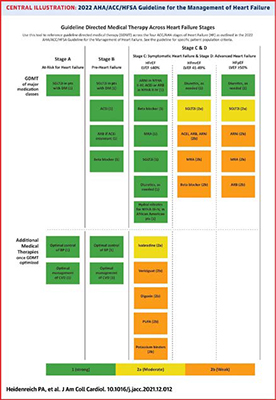
The COVID-19 pandemic has highlighted the need for alternative approaches to care delivery for patients with advanced heart failure, including telemedicine. Heart failure is a chronic condition characterized by the inability of the heart to pump enough blood to meet the body's needs, leading to symptoms such as shortness of breath, fatigue, and leg swelling. This condition affects millions and often leads to recurrent exacerbations and hospitalizations. Traditional management of heart failure involves regular visits to a healthcare provider, medication management, and lifestyle modifications. However, patient non-compliance with guideline-directed medical therapy (Figure 1) and failure to optimize hemodynamics can lead to poor patient outcomes.
Telemedicine can also facilitate communication between patients and healthcare providers, exchanging important information and allowing for adjustments to treatment plans as needed. As a result, providers have been increasingly using telehealth services to care for patients with cardiovascular disorders. Remote monitoring of heart failure patients can improve diagnosis and treatment accuracy and timeliness.
In managing heart failure, telemedicine has several applications. Remote monitoring involves using wearable devices or home-based monitoring systems to collect real-time data on a patient's vital signs (e.g., blood pressure, heart rate, heart rhythm) and other physiological parameters. This information is then transmitted to a healthcare provider, which allows healthcare providers to monitor patients remotely and collect data without requiring them to visit a physical medicine facility. For example, CardioMEMS (Abbott, GA) is a wireless monitoring system implanted in a patient's pulmonary artery to measure pulmonary artery pressure in patients with heart failure. Healthcare professionals can remotely monitor the readings and modify treatment plans, with published data showing decreased hospital readmission rates. Similarly, implantable cardioverter-defibrillators (ICD) can remotely monitor the device's function and detect abnormal heart rhythms, sending reports to monitoring providers to intervene. Remote EKG monitoring devices (e.g., LivCor, AliveCor, etc.) are another example of telehealth and telemedicine. This technology allows patients to record ECG (electrocardiogram) tests from their homes using a wearable device connected to their smartphone. Data collected by the device is sent to healthcare providers, who can use it to diagnose abnormalities.
Tele-education involves using technology to provide educational resources to patients with various cardiac conditions, including videos or webinars for self-care strategies. Tele-consultation allows patients to receive care remotely from a healthcare provider, nutritionist, physical therapist, or nurse coordinator without an in-person visit. In patients with advanced heart failure and many other ailments, remote technologies have aided in connecting with other patients using virtual 'rooms' to discuss their conditions and treatment plans to help support each other through their journey.
Increased utility of remote healthcare services during COVID–19 revealed numerous advantages: controlling the spread of infective illnesses, pre-screening patients before in-person visits, reducing physician burnout, diversifying practice patterns, preventing germ exposure to vulnerable populations (e.g., chronically ill, pregnant, elderly, or immunocompromised), maintenance in the continuity of care, and enhanced the protocolization for data collection and interpretation).
Despite the numerous potential advantages, telemedicine does have its limitations. Some significant challenges include patient familiarity with technology, reliability of remote technology, healthcare data breaches, and absence of physical examination. Furthermore, lacking human touch limits the patient-provider connection, which could be a potential cause for unearthing mental health issues and a greater need for future counseling.
Currently, there is a lack of standardization across telemedicine platforms, making it difficult for healthcare providers to use multiple systems and for patients' participation. Regional variations in telemedicine regulations make them challenging to understand and may increase providers' complexity in adhering to telemedicine regulations. Furthermore, some telemedicine solutions could be insecure, and providers may be concerned that patient privacy cannot be maintained. Telemedicine use can also be made more difficult by a lack of compatibility with electronic health record systems. Telemedicine technology and equipment rely entirely on hardware and software, requiring extra support and training for employees or caregivers. To tackle some of these hurdles, low cost of equipment setup, redundant patient safety features, and standardization of electronic health records may increase the utilization of telehealth and telemedicine.
The outlook for telemedicine in healthcare is positive. With the proliferation of wearable technologies and the increasing adoption of electronic medical records, telemedicine will continue to play a significant role in managing cardiovascular conditions. As more providers utilize remote healthcare technologies, increasing adoption into other specialties may offer a new method for delivering equitable healthcare to patients in need.
References:
1. Kane, Carol K, and Kurt Gillis. “The Use Of Telemedicine By Physicians: Still The Exception Rather Than The Rule.” Health affairs (Project Hope) vol. 37,12 (2018): 1923-1930. doi:10.1377/hlthaff.2018.05077
2. Shaver, Julia. “The State of Telehealth Before and After the COVID-19 Pandemic.” Primary care vol. 49,4 (2022): 517-530. doi:10.1016/j.pop.2022.04.002
3. Angermann, Christiane E., et al. “Safety and Feasibility of Pulmonary Artery Pressure-Guided Heart Failure Therapy: Rationale and Design of the Prospective CardioMEMS Monitoring Study for Heart Failure (MEMS-HF).” Clinical Research in Cardiology, vol. 107, no. 11, 2018, pp. 991–1002., doi:10.1007/s00392-018-1281-8
4. Shavelle, David M et al. “Lower Rates of Heart Failure and All-Cause Hospitalizations During Pulmonary Artery Pressure-Guided Therapy for Ambulatory Heart Failure: One-Year Outcomes From the CardioMEMS Post-Approval Study.” Circulation. Heart failure vol. 13,8 (2020): e006863. doi:10.1161/CIRCHEARTFAILURE.119.006863
5. Heidenreich, Paul A et al. “2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Journal of the American College of Cardiology vol. 79,17 (2022): 1757-1780. doi:10.1016/j.jacc.2021.12.011